According to the statistics of the World Health Organization, breast cancer is currently the cancer with the highest incidence rate in women, and its fatality rate is also quite high. In routine practice, the early treatment of breast cancer is neoadjuvant systemic therapy before surgical resection, such as chemotherapy, targeted therapy, immunotherapy, etc. These treatments can help downsize tumors and improve the prognosis of those patients being treated. Therefore, the present study collected the data of breast cancer patients from the Kaohsiung Medical University affiliated hospitals in the past ten years, and found that only 17.2% patients had a pathologic complete response (pCR), but most patients (about 82.8%) still had in situ residual cancer cells after the neoadjuvant systemic therapy.
Breast cancer patients had different clinical characteristics, such as clinical stage, type of breast cancer (hormone receptor) and cell type, and different imaging characteristics on contrast-enhanced computed tomography, such as tumor size, shape, contrast enhancement and textures. These variety of factors may together influence the treatment outcome of neoadjuvant systemic therapy. Therefore, the present study integrated both clinical and radiomic features to establish a more accurate prediction model for pCR using an artificial intelligence-based machine learning technique. The results demonstrated that the predictive accuracy of the “integration model” (87%) was significantly higher than that of the "clinical model" (69 %) and the "radiomics model" (78 %). Therefore, with the assistance of prediction model, it will be helpful for clinicians to more accurately evaluate the treatment outcome prior to the therapy, and to adjust the treatment regime for improving the prognosis in patients with breast cancers.
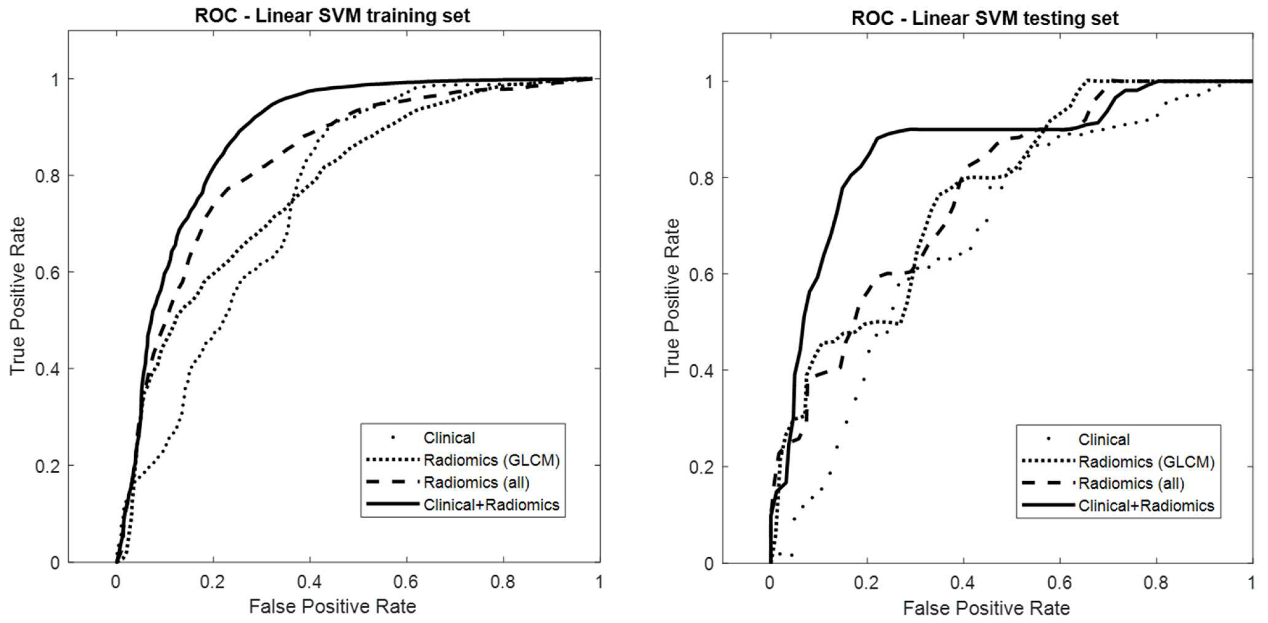
Left: The receiver operating characteristic curves of clinical, radiomics, and integration (clinical + radiomics) prediction models using training dataset.
Right: The receiver operating characteristic curves of clinical, radiomics, and integration (clinical + radiomics) prediction models using testing dataset.
Application and Highlights:
1. Integrating clinical and CT-based radiomic features can help improve the accuracy of predicting patients' response to pretreatment.
2. The type of breast cancer (hormone receptor), shape, size, and the subtle texture changes of the tumor played important roles in the prediction model.
Research Team Members:
Huei-Yi Tsai, Tsung-Yu Tsai, Chia-Hui Wu, Wei-Shiuan Chung, Jo-Ching Wang, Jui-Sheng Hsu, Ming-Feng Hou, and Ming-Chung Chou
Representative Department: Center for Big Data Research and Department of Medical Imaging and Radiological Sciences, Kaohsiung Medical University. Department of Medical Imaging, Kaohsiung Medical University Hospital.
Introduction of Research Team:
The team has been committed to combining artificial intelligence and medical image analysis to improve medical quality.
Contact Email: mcchou@kmu.edu.tw
Publication: Tsai H-Y, Tsai T-Y, Wu C-H, Chung W-S, Wang J-C, Hsu J-S, Hou M-F, Chou M-C. Integration of Clinical and CT-Based Radiomic Features for Pretreatment Prediction of Pathologic Complete Response to Neoadjuvant Systemic Therapy in Breast Cancer. Cancers. 2022; 14(24):6261.
Full-Text Article: https://doi.org/10.3390/cancers14246261